These learnings are only provided as practical suggestions from my personal experience of diagnosis/surgery, chemotherapy, radiation, and long-term impacts. Please make sure you speak with your medical team about what you need and how best to support you.
How I maintained sanity between diagnosis and surgeries.
Project managing chaos
Despite being an experienced project manager of big complex problems in my day job, I felt like I was down a well screaming in the dark at all the people, processes and computers that seemed to be intent on finding creative ways to say “no”. It feels like the cruelest episode of ‘Candid Camera’ having to play what is likely the worst day of your life on repeat to every insensitive robot on the other end of a phone. All that I needed was an answer to what the hell do I do now about x or y, and all I got was another request for another form or another repeated explanation of “I’ve just been diagnosed with cancer”.
In a crisis, people tend to do one of two things – bury the emotions and focus on cold hard facts and tasks or fold up into the fetal position and hope that the bad dream will end.
I opted for the task-focused option and treated it a like a work project. I had a number of people who presumed that I was just sitting at home binge watching Netflix in between diagnosis, surgery and chemotherapy…they were clearly the optimists among us. Reality felt more like me trying to organise 20 Greek weddings in a tsunami.
So, in the two days I had between diagnosis and going in for surgery, I opted for retail therapy - I went into Kmart and headed straight to the stationery section.
My project management tools:
A zip-up folder to keep all current medical information and records that wouldn’t spill open if I ever managed to drop it.
A second folder to use for background information/historical records once hospital procedures/tests/appointments had been completed.
Plastic inserts for both folders to keep lose documents and all records from different appointments/specialists together.
A writing pad to take notes during appointments and phone calls (always a good idea given that you end up only taking in/absorbing half of what is actually said most of the time).
Pens, highlighters, and sticky notes for the never-ending supply of forms and to keep myself focused on key information from all the booklets and prints outs.
After each appointment with a new specialist etc, I would sticky tape their business card to the inside cover of my folder so that I had them for easy reference every time I was asked who was treating me for what (and for all the damn forms!).
Organise/file whatever you can (the BCNA Journey kit provides a great bunch of resources that also help you do this). My folder had things like results from blood tests, scans, pathology, and referral letters. Also, you’ll need the folder to be big enough (A4+ size) to bring any radiography images with you to all appointments.
Personal admin:
The type of government, work, finance and health agencies that need to know what's happened builds up. You'll need to think about:
Insurance companies - income protection, life insurance, health insurance.
Human Resources teams at work to keep track of sick leave entitlements and to assist with accessing work-related supports such as negotiating time off and return to work.
Salary sacrificing arrangements like car leases that may need to be suspended if under novated lease options while you're not at work.
Australian government agencies like Centrelink if you're applying for disability/sickness benefits; Australian Tax Office if you're applying for early access to superannuation (there are a myriad of hurdles to jump through, but get onto it quickly to find out if you are eligible).
Private health insurance companies will need to know everything so they can advise what your likely coverage will be.
Navigating the health system comes with two challenges: the terminology and the bills. The bills will add up quickly, even if you have private health cover. I found out the hard way that in-hospital expenses (when you're admitted as a patient for a procedure or surgery) are reimbursed by both private health AND Medicare. You end up jumping through 100 hoops to get one paid invoice processed for a refund - registering at Centrelink, filling out dual/two-way reimbursement forms that are not (as at this date) able to be processed online, and lodging them in person or mailing them. Private health cover usually does not apply to out-patient expenses, like CT scans, bone scans, or pathology tests. These are often able to be claimed on the spot from Medicare at the health provider, but again, you may need to lodge them online, so there is a long wait between paying the bill and receiving a refund. Not to mention the out-of-pocket expenses that are incurred due to Medicare schedule fees being waaaaay out of touch with the current health service fees.
The number of forms and email correspondence builds up very quickly, so you’ll need to set up your very own make-shift medical reception office at home:
Categorise emails so that when you need them, you can find them.
Scan everything you send in snail mail (STILL in 2018, computer says no, it needs hard copy).
Buy a printer and scanner and pre-buy express mail envelopes – you’ll be having to sign and send through consent forms on the same day sometimes when things are moving so quickly.
Get a good old fashioned wall calendar to keep track of all your appointments and so that anyone else at home can see where you are supposed to be (I put up the Guide Dog version on the wall but still bought the 2018 QLD firefighters version… in the spirit of fundraising of course ).
Delegate information disclosure to family or a friend if you think you won’t be able to talk to the insurance company etc or are feeling overwhelmed – these will be forms you can get from agencies directly.
Packing for hospital:
For hospital stays, I would again suggest going into shops like Kmart or Target etc where you don’t need to spend a lot of money on items you will likely throw out in months to come (comfort first, couture later!). You’ll want an arm load of track pants, t-shirts, zip up jumpers, singlets and PJs, not to mention some creature comforts like a big fluffy dressing gown and slippers. And an overnight bag for admission. Hospitals are cold but can also feel quite stuffy so best to pack for layers.
Also, you want to get loose clothing, particularly tops, due to the pain and swelling post-surgery. Zips are good because doctors and nurses can just get right in there when they’re checking on you (especially the four-hourly wake ups when you’re half asleep from the drugs and you’ve got someone poking and prodding you).
For breast cancer, you’ll need special post-op bras (no wire, front-opening) because you need to wear them 24/7 for at least the first week or two after surgery to keep swelling risks down and to reduce pain. A light adjustable shoulder bag and L-shaped pillow are also a necessary accessory if you end up with surgical drains. Breast cancer nurses will often provide you with these, but always good to have a second one. The pillow comes in handy for sleeping and while in the car when you'll be feeling every bump from all the future council pot-hole fixes needed.
When you get home from hospital:
Do not underestimate how quickly you’ll get tired. Some cheat sheet things I did included:
Facewipes (baby water wipes) for night time /morning – two showers in one day can take a heap of energy from your reserve so just focus on one and do your own version of a sponge bath.
Listen to your body – rest, don’t fall (get to know your limits) – your brain says yes but body will have other ideas.
If you can, arrange for meal deliveries, or ask a friend/family member to come over and help cook up a storm and freeze stuff – soups, casseroles, protein balls, savoury mince – it's easy to add an egg for a quick protein hit. Smoothies are ok too as long as you are pumping it up with good quality protein.
Don’t try and play home hostess – ask for help with house work and shopping. Try grocery deliveries and even some home cleaners.
Think: Essential Organs Only. Like with a car crash victim - the body will pump blood to essential organs; it doesn't matter if your limbs fall off! Pace yourself and your energy output when it comes to keeping in contact with everyone - calls/texts, visitors. As much as they are all well-intentioned, it will drain you. Ask someone else to send general update messages on your behalf. Let people know in advance that you may be on ‘radio silence’ for a few days/week and that you’ll respond when you can.
Above all else, focus on quality – food, sleep, support. Your body will have been hit from all angles, not just the emotional toll of the diagnosis but also the cumulative effect of general anaesthetics, pain medication, and surgery. You need to nourish and nurture your body, and that includes sleep. If your doctor is ok with it, try natural sleep supplements or opt for sedatives in the early days when you can’t distinguish between tired or wired.
And find a way to process whatever it is you're feeling - talk to someone, read, write, meditate, ask someone to drive you to the beach. Despite many voices of support and hands to hold, this can feel like the loneliest path to walk. But if your mind is strong, your body will follow its lead.
How to predict the unpredictable of chemotherapy.
Planning for 'just in case'
My blog post, Chemo: Friend, not Foe, includes some broader reflections about how I managed chemotherapy. But there really is only one starting point - keeping your mind in a state of balance is critical to helping your body deal with whatever may come. And when I say balance, it includes embracing the fear, anxiety, and anger you may be feeling. But it absolutely must also include nourishing and nurturing your mind and body, inside and out.
I did all I could to feel prepared for the physical impacts of chemo treatment. As for preparing for how I might feel with every other experience and side effect, I chose to be open to asking for help and constantly surprised at the wonderfully random sources of support that are offered.
Before treatment: Prepare your home and your self
Similar to the earlier learnings about surgery/hospital, prepare as much as you can beforehand. That includes Master-Chef'ing your kitchen and preparing some easy meals that can be stored in the freezer. It also means getting rid of whatever you won't need, that won't serve you well, such as comfort food, hair care products, and alcohol. Either donate to friends/family/charity, or store it for when you are ready to use it again.
Clean and clear your bathroom cupboard, pantry, and clothes collections - you may need someone to help care for you if you experience severe fatigue like I did, so it's easier if they know where your sloth clothes are, can access readily made meals, and can easily find medications etc.
Create a chemo 'go-bag' that you can just pick up and take with you each session. Mine includes phone charger (for the long days/appts), beanie/socks/scarf (it can get cold in the clinic), water bottle, headphones, book, journal, lip balm, hand cream, antibac mini, tissues, travel calm wrist bands, ginger lollies. I usually wear layers given that pre-meds like steroids can cause facial flushing.
Prepare a germ-free zone as best you can - I always change my bed linen and towels before each session and give the house a full work over. I've also had to get used to asking others to help me do that during treatment cycles when/if energy levels are low and to prevent exposure to too much chemicals. Plant-based cleaning products are much gentler on the body given the chemo will lower your immune system.
Work out a schedule for bathrooms if you share it with others - chemo drugs are by nature toxic, so others need to be careful about sharing the bathroom in the first 4-5 days post-treatment. They also need to protect you from themselves, including washing hands and embracing the joys of anti-bacterial hand wash. I have three placed around the house - bathroom x 2 and kitchen.
The chemo clinic you attend should conduct a pre-admission session to take you through the ins and outs of your treatment, but if not, write down any questions you have and ask your doctor or a nurse when you go in - your memory may not remember everything!
Day of treatment: Be your own best friend
Despite all the information and preparation, I still went through massive anxiety swings before walking into the chemo clinic. Part of what helped me to re-focus was the heart ultrasound (usually conducted before you start chemo to make sure your heart is ok). The art of breathing and thinking slowly will help in among a world of busyness. If you can, take a friend or family member with you. It can be just as confronting for them seeing you attached to IV drugs, but if you are there on your own, be sure to talk to the nursing staff about anything - there is no such thing as a stupid question.
I usually avoid caffeine before treatment, and have something light to eat like scrambled eggs (depending on your appointment time).
If you have a port-a-cath for the IV drugs, wear something with a v-neck or zip to allow the nurses easy access, depending on where it has been placed on your chest. You may also want to invest in some Emla cream - you can get it from the chemist. It is a local numbing cream so if you apply some over the port area an hour before your treatment, it should help the needle sting !
Write down any advice and instructions from the pharmacists/doctor/nurses about the medications that you may take home, including steroids, sedatives and anti-nausea.
The steroids can cause you to feel a little wired by the end of the day so make sure you take the sedatives and go to bed early.
After treatment: Ride out the roller coaster - it will end
People had told me chemo was like the combination of the worst hangover and flu you’ve ever had. That’s probably accurate in concept, but just played out on a roller coaster ride. The first day after treatment, I didn’t really feel anything different. The second day, my thoughts and legs felt a little wobbly. Day 3 was, as the nurses had predicted, when things changed. By then, the medication was doing its job and basically hitting the reset button in my body.
Keep a diary of your first round – side effects, what you ate, drugs you took, energy levels out of 5, water intake, exercise, etc – in part to monitor for nurses’ report back next session, but it will also help to reduce anxiety about future rounds and feel some sense of predictability.
I start each morning with a protein smoothie before I even get out of bed (this is where I need someone to get it for me because I can't easily make it down the stairs). It can help with any nausea and energy in the morning. I also keep snacks like rice crackers and jelly beans on my bedside table.
Easy does it with exercise - sometimes, a trip to the corner or down the driveway is worth celebrating. Other days you may need to just stay on the couch or in bed. Then energy levels will pick up again and you can find the pattern that works for you.
Keep a chair in the bathroom in case you feel weak after a shower.
Be aware of what you put in and on your body - use low tox/chemicals where possible for all skin care - you will need to moisturise every day as skin can become quite dry from the treatment (e.g. try baby products or hypo-allergenic skin care products for body washes and creams). Where you can, opt for organic and fresh vegies/fruit, especially if you are putting them raw into juices or smoothies.
I use black nail polish and a nail strengthener on my finger nails and toes to prevent UV damage that may otherwise cause nails to lift.
Be gentle with your digestive system - chemo will stop everything moving, so invest in some natural digestive tablets like Nulax.
Water water water ! Flavour it with pressed juices or lemon but try and avoid sugary cordials. Aim for 2-3 litres a day.
Be prepared for your taste buds changing - for example, I cannot handle tea or sweet stuff. Instead, am craving spices and salt. There is a metallic taste that will likely build up over time and/or in between chemo rounds.
Do not fear the scales ! The chemo nurses will weigh you in each session, so there is no need to beat yourself up. Focus on any weight loss goals after you’ve been through the treatment/fatigue. If you’re eating well/healthy, you should be burning what you’re eating on those low energy days. When there's a good day, walk, yoga, pilates, gym, whatever helps keep you moving. But balance it with rest when your body needs it.
Buy in the help / support you need – sometimes you need to separate the family/friend support, including counsellors, naturopaths, homeopaths, acupuncturists – tools to help your body sustain the treatment (eg, build immune system support, energy/fatigue, emotional guidance to help navigating the tsunami of feelings).
Take the good with the not-so-good:
Be honest with what you can and can't do when it comes to communicating and catching up with people, particularly during the 'low immune system' period. Friends and family will understand if it takes you a day or a week to respond - just give them a heads up beforehand that you may be off the radar for a while.
Use puzzle books, or just puzzles, whatever to keep your brain active – chemo brain fog is real. And if you're not working, find ways to stay connected if possible so there's not such a huge gap when you go back later.
Do things you would not normally do – water colour painting, wooden spoon carving, writer's course, cooking !
Balance self help books with escapism/fun – it does not have to be serious all the time.
Plan short trips/overnights when you have a pattern of side effects/energy you trust (knowing it can change, so check on cancellation policies).
Ask your friends to send you pics of their holidays, their view from the office – whatever it takes to get you out of cabin fever. Or ask someone to take you for a drive somewhere (take a pillow and blanket in the car) to get another view other than your own four walls.
Work through your very own 'happy happy joy list' for your good days that get you out of the house, like trying a new coffee shop, going to an event or workshop that taps into your creativity. Then also include tv shows, movie marathons, and books for low energy days when you just need to rest at home. Ask someone to read to you if you cannot concentrate – there’s a reason why we loved it as kids !
Celebrate the milestones, whatever you make them. Go to your fave brunch/lunch spot, buy a cold press juicer, order that skin care indulgence, and plan for a holiday or a break somewhere when you have eventually finished your treatment.
Above all else, be kind to yourself.
Dealing with the practical side of hair loss:
There's no easy way to prepare for how this will feel for you. All I offer is the strategy I took to try and reclaim some decision-making in what otherwise feels like you're a passenger in it all. There is nothing to be gained through welcoming denial - it's one of the most feared side effects of chemo but just about everyone will experience it. My approach really helped to reduce the shock of losing my hair when it finally came because I felt like I had at least controlled the in-between stages.
I've also included a link on the 'Info' page about how one woman documented the timeframe between losing and regaining her hair.
A few weeks before I started chemo, I had my long hair cut off into a pixie cut (short back and sides). Hair salons will sometimes offer a private room, or if you can, like me, some hair dressers work from home so it's a lot more private.
As predicted, my hair started to fall out 2 weeks after my first chemo session. I knew the warning signs, like sore scalp and feeling itchy, so when the first follicles came off in the shower, I asked a friend of mine to shave my head to a no. 2 buzz cut.
I wore a soft cotton cap to keep my head warm and to collect loose hairs that would ultimately fall out over the next week.
Again, use low tox/organic products on your head - I use organic baby shampoo products to wash my 'hair' (fluff !) and moisturising cream to reduce red and dry skin taking over.
Find ways to feel pretty – ask someone you trust to go shopping for a wig, look at alternatives like 'fake fringes', scarves, hats etc – get them before hair loss. And shout yourself a new outfit, new shoes, big earrings, jewellery, something with colour, and silky PJs when you can't be bothered showering.
Stores like Starkles (online as well as in Brisbane and Gold Coast) offer a whole range of headwear that doesn't make you feel like a chemo patient ! My absolute best buy so far was a fake fringe that I can wear under hats or caps and it fools EVERYONE !
Hospitals and breast care support centres may also offer wig libraries where you can 'loan' a wig rather than buy one (they can be up to a few hundred dollars to buy) so make inquiries with your local chemo clinic or cancer support programs.
Your eyelashes and or eyebrows may also fall out/break or just thin out over time. Be careful with eyelash extensions - make inquiries about organic eyelash products and glues as there are risks with allergic reactions, and your skin will be more sensitive than usual.
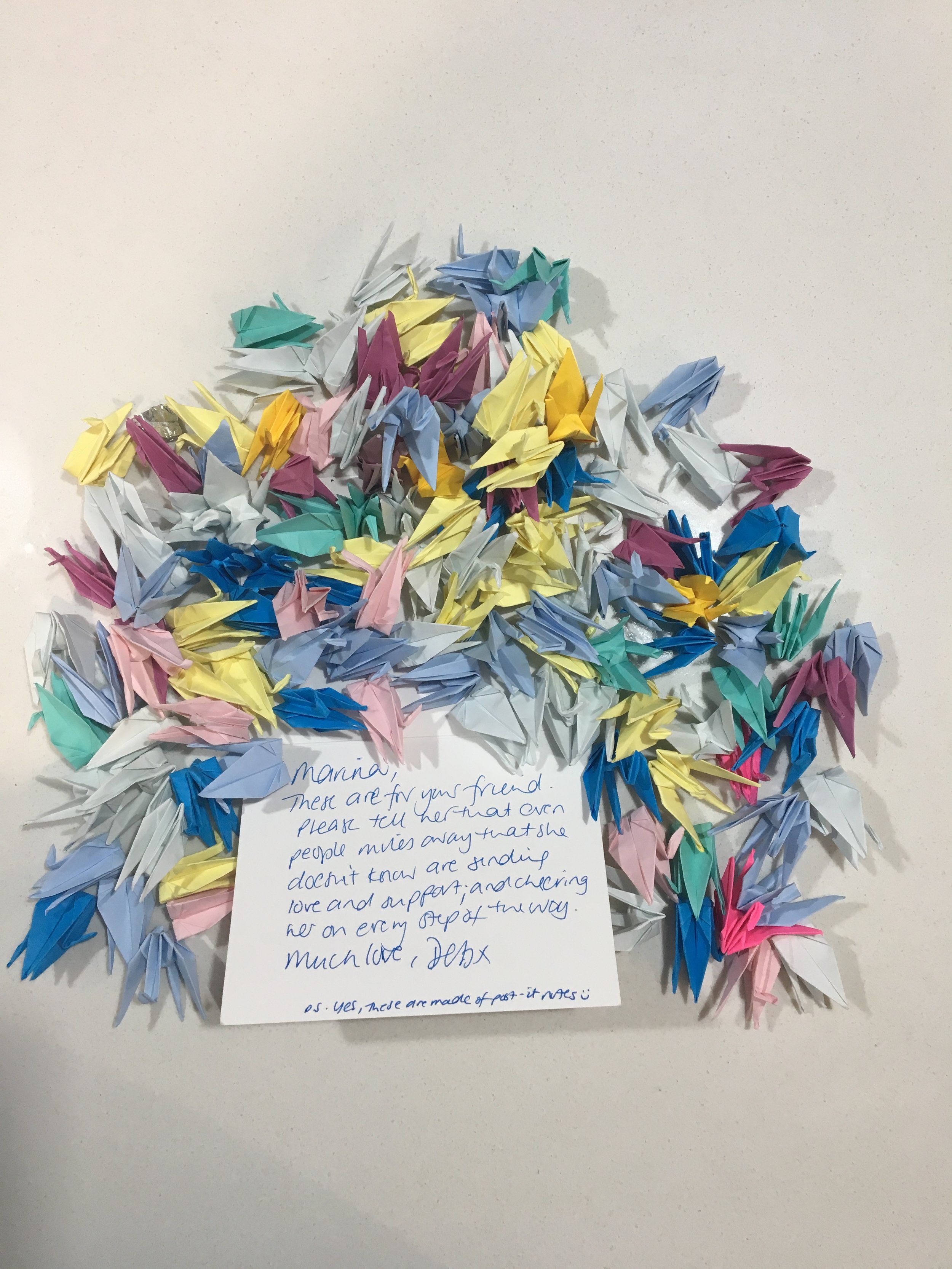
These images of Icon Cancer Centre at Wesley Hospital in Brisbane are an example of how a paper crane project generates support for me and everyone else who walks through the doors...some have come from the other side of the world (through my friend, Marina) made by people I will never meet.
The daily meditation of radiation.
Just breathe
By the time I finished my 12 rounds of chemo, radiation seemed like a pretty simple task: lay down, don’t move, and breathe. Usually for breast cancer, there’s a 16 (3 weeks) or 30 (6 weeks) daily treatment program (Mon-Fri.) It depends on how extensive the cancer was. How they do it also depends on which side/where the cancer was. In my case, the tumour was on the left so I was treated using a deep-breathing technique to try and protect the heart a bit more.
For me, radiation was a slice of peace and quiet and felt almost like a medically-induced meditation. Even if I had been rushing around between other appointments that day, or stuck in traffic, or had 260 other things on my mind, it was my time to just focus on my breathing. It was about 15 minutes of me, a [bloody] big machine, listening to some cool music in the background that would keep me in a state of enforced mindfulness.
The planning session
Before you start your daily sessions, you spend a few hours in the radiation clinic for a planning session so that the radiation technicians and oncologist can carefully map out your treatment. Here’s a few pointers to help you that day:
You need patience. Radiation is an exact science and a highly complex one for good reason - teams of physicists and radiation technicians measure to the millimeter where the radiation beams need to go to ensure they treat the area where the cancer was/is. This usually includes reviewing any x-rays, CT scans, mammograms, ultrasounds and other pathology reports to record exactly where the treatment area is.
Learning new ways to breathe. If you are having treatment on the left side, you may be asked to trial a deep-breathing technique aimed at moving the heart muscle just enough out of the way to reduce any long term risks of damaging your heart. If you’ve had a CT scan before, it’s very similar. It usually requires you to hold your breath for up to 20 seconds. During the planning session, you’ll have lots of practice runs.
You’ll get tattooed. Tiny dots are placed on your body around the treatment area so that the radiation technicians know where to line up the lasers during treatment. I had three - one on each outer side of the breasts and one in the middle of my sternum. These will sting - a lot ! But only for a few seconds. They are permanent marks too, usually blue/green in colour, but very tiny.
Practice your inner zombie pose. The staff will need to move you around a fair bit on the bed to get the positioning perfectly correct, so you may feel like a zombie while you lay still and they pull you/the sheet you’re laying on to the left or right, or up and down. For my treatment, I laid on my back and my arms were placed above my head, so I had some discomfort from the scar tissue/stiffness as a result of previous surgeries. Work with the staff to make sure you’re able to hold the position for at least 15 minutes. The staff will usually then use a transparent film to hold over the treatment area of your body and mark up the measurements - these plans get entered into the computer for the medical specialists to review and confirm the plan before your first treatment session.
First day
Some people get very anxious about radiation, and like everything else, the first session can feel quite overwhelming and clinical. But that’s because you’ve got a massive machine moving around you making humming noises while you lay frozen alone in a big cold room… so it’s understandable to feel a little freaked out ! Having said that, the first day is always the hardest, but after a while it becomes part of your daily routine.
Remember: it doesn’t hurt. You don’t feel anything while the radiation treatment is happening.
There will always be at least two radiation technicians in the room to set you up. Once you’re on the bed, the technicians will help move you to make sure your body is in exactly the right position to ensure the lasers line up with the tattoos that you had during the planning session. You’ll hear a lot of numbers/measurements being called out between the staff as they run through where you need to be positioned. The bed you’re on may also move up/down/left/right. Set up takes about 5-10 minutes, depending on your treatment area.
The staff will get the machine to do an X-ray first before the radiation starts - this will confirm that you’re in the right position according to the plan.
Treatment can take about 5-10 minutes. During this time, the staff are outside the room watching from the cameras and will speak to you through speakers. The machine moves around you to provide radiation treatment from both sides of your body. The machine can sometimes come up quite close to your body or face, and can be a little intimidating, so think about taking an eye mask with you or just close your eyes. If you are doing the deep-breathing technique, you may have eye goggles that help to provide visual cues for your breathing, so you won’t see anything anyway.
Check with the staff during set-up about how to get their attention during treatment, such as having an itchy nose, needing to cough, or moving your arm/leg if it gets a cramp - they may not be able to hear you but they will be able to see you.
Booster sessions
With breast cancer, you can also have ‘booster’ sessions towards the end of your treatment - these are designed to specially target the area of the tumour. For example, I had a 30-session cycle: 25 full sessions that covered the entire left half of my chest, and 5 boosters.
Boosters will still ‘burn’ the area of the radiation, but are confined to a much smaller area. You can leave dressings on surrounding areas during these last 5 sessions.
The subtleties of side-effects
Like chemo, everyone responds differently to radiation. Side effects will also be different depending on what type of radiation you have and how long the treatment goes. Hair loss, skin burns and inflammation, and swelling can occur along with other issues like nausea.
For breast cancer, the biggest issue is usually the impact on the skin for the chest area (addressed below). But fatigue is also quite common. I asked for my treatment sessions to be scheduled in the afternoons so that I could get to gym, appointments etc, in the morning and then just go home and rest after treatment. But other people may go in the morning and head straight to work but need to come home early if they feel their energy is fading.
Over time, fatigue can build up, but it’s subtle - not like chemo. I drove myself to and from the hospital every day until the last few days of the 6 week cycle when I didn’t feel comfortable driving anymore because my reaction time/concentration was slowing down.
Even after you finish radiation, the treatment impact continues for up to two weeks, so be prepared for fatigue and other issues like any skin burns to extend further than you last treatment session.
Skin care
Breast cancer radiation treatment usually covers half the chest area, and comes right up to the skin surface. This requires a regimented daily skin care routine to prevent and manage the burns to the skin that will build up over the course of treatment. Some women may prefer to try medical products that are applied to the skin and act like a second skin - your medical team will discuss whether this is appropriate for your treatment.
For me in the first 1-2 weeks, the skin became increasingly red and looked like a minor sunburn. But during weeks 3-4, the redness and swelling increased. By weeks 5-6, some sections of the skin had blistered and broken, which required daily dressings and reviews by the nurses. One of the staff described the skin as fragile as ‘wet tissue paper’ at this time, so home-care is critical to taking all the steps to protect the skin, especially the areas that may have broken. Using basic dressings can cause damage as they are removed by taking bits of skin as you peel them off, so you’ll have to trial a few different ones with the nurses to suit your skin.
Dressings usually need to be removed prior to each treatment session, so bring them with you to the hospital and any creams you are applying. Radiation preparation requires the skin to be dry, so don’t apply any creams/gels etc a few hours prior to treatment. You’ll need to be prepared to reapply creams and dressings 3-4 times a day. The treated area will feel very warm and sore (just like bad sunburn), so you may also want to experiment with cold packs over your clothes to help relieve the heat and swelling/sensitivity.
Swelling can occur for a month or more afterwards, so make sure you stay in regular contact with a physiotherapist to reduce your risk of lymphodema. The burns/redness will usually reduce after the first few weeks, but sensitivity can continue for longer.
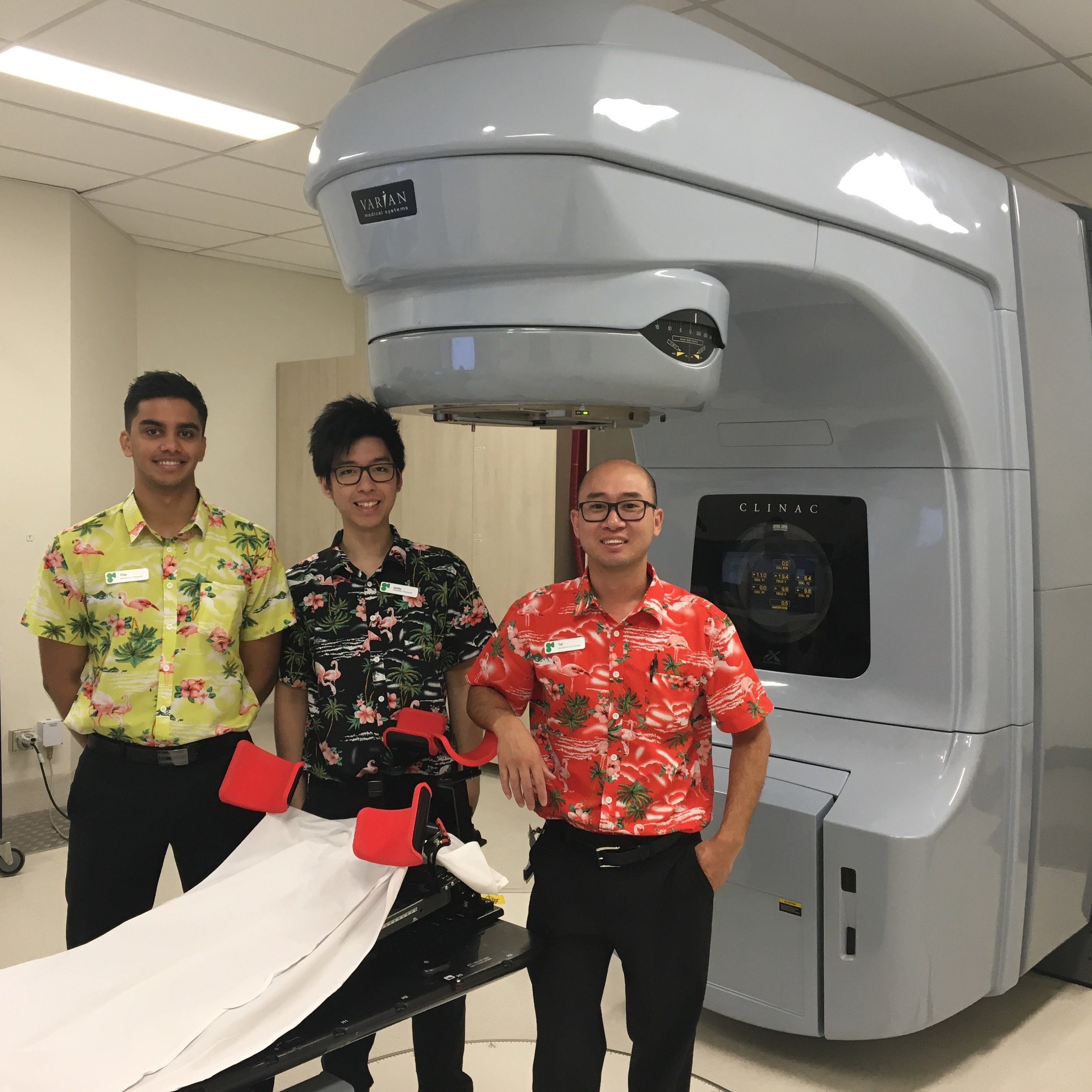
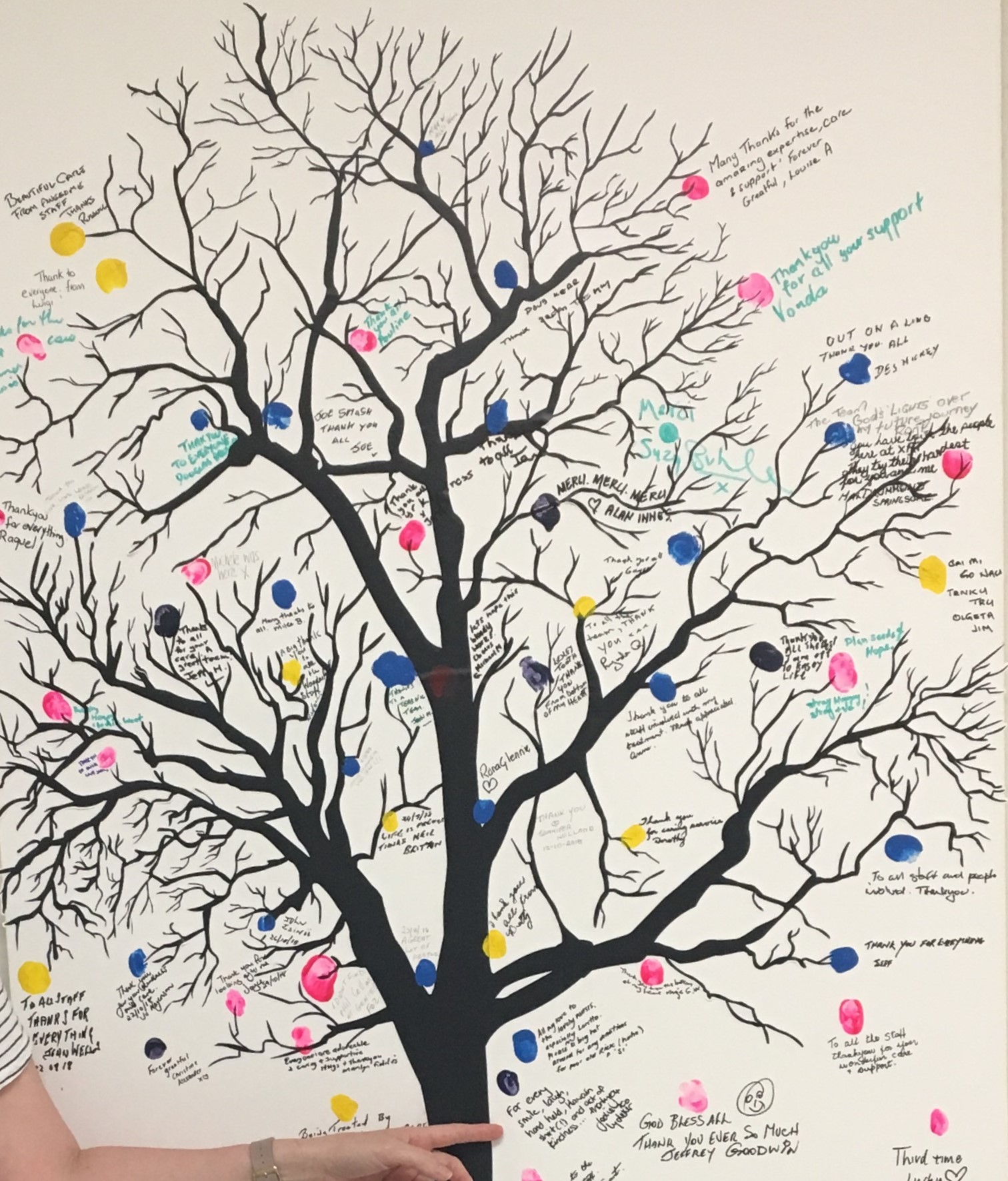
My favourite day was Friday when the Genesis Cancer Care nurses and radiation technicians would wear their Hawaiian shirts (pictured above) just to help all of us escape to a day dream. The Genesis clinic at Wesley Hospital in Brisbane also has a beautiful way to mark the end of treatment … mine says: For every smile, laugh, hand held, Hawaiian shirt (!) and act of kindness …thank you.
Managing longer-term impacts.
The treatment hangover
If you’ve also had chemotherapy in addition to radiation, your body will be dealing with the cumulative impact of both treatments. This will wreak havoc on your immune system and energy levels. Combined with potentially also surgeries, your body has been through the wringer(!), so try not to plan too much in the period immediately following your last official treatment. I received sage advice that energy levels can feel like a merry go round for 2-3 months, and it was pretty accurate! Any celebratory holiday planning should be done cautiously … opt for day spa retreats or beach-side escapes rather than skiing or mountain climbing in the first few weeks/month after treatment.
Emotional hang-overs are also quite common and can bite you on the proverbial backside when you least expect it … My blog post on delayed grief was about this (I called it post-traumatic treatment disorder). Take the time to factor this into any return to work planning / return to ‘normal’ planning. If you haven’t already connected with emotional support services, either individually or as a group, you may find a proactive approach beneficial to help you process all of what your body has endured.
When you do finally ride out the first few months of physical and emotional hangovers, be sure to gift yourself a holiday anywhere in the world before you plan your return to work and ‘normal’ activities ! You need to start with the presumption that your real recovery period is the same length as your treatment period. So… 12 months of treatment = 12 months of recovery. In that time, you can figure out what your ‘new normal’ is…
Returning to Work.
First day of work ‘to do’ list
My experience returning to work fell a little short of expectations – mostly my own expectations about thinking it was going to be all smooth-sailing and emotion-free … and it’s still tricky 2 months on (read my blog post here). But there are some practical things I’ve identified below that would have taken the edge off. It most definitely requires some pre-emptive action the week or so before to get your boss and HR team across what is important for you.
An email in advance setting out a structure for the morning including facilities/orientation, HR, IT, someone from your team to do a mini-orientation.
Build in a coffee break or two to allow you to clear your head in between any induction/on-boarding sessions.
Arrange a known colleague to meet you when you first arrive if you boss or HR person is not otherwise available.
Personal logistics such as a locker key and security pass allocated upon arrival.
A designated quiet room that has been pre-booked/reserved for the first day or two (if you don’t have an office). You may feel very exposed to the constant ‘attention’ that will heighten any existing emotional anxiety/stress.
A designated contact person/’buddy’ in your team to assist settling in for the first day or two, and to be available to do a team-specific computer/system orientation
A designated HR officer as a primary contact for broader support during the first week or two.
A designated IT/support officer to assist with basic set up etc.
A reminder about how to contact personal support services.
Depending on the flexibility of workplaces, it is well worth considering part-time hours or amended start/finish times for the first week or month. The issue may not be the physical toll of your workplace, but the brain-drain from having to concentrate and focus and string more than two words together after a significant time away will almost certainly contribute to physical fatigue.
A few other things I’ve implemented to help with getting the balance right is:
Getting healthy meals delivered every week to give me less excuse to miss lunches or make bad (emotionally-driven!) food choices
Committing to exercise on my days off and weekends if I’m not feeling up to the gym etc after work.
Arranging a cleaner every 3 weeks to do a ‘big clean’ in between the usual weekly cleans so that I’m not wasting all my ‘me-time’ on domestics !
Breaking up the work week – e.g. work Mon and Tues, off Wed, work Thurs & Fri. Build up gradually to any full time workload.
And most importantly: Don’t rush to get back to a ‘normal routine’ – your most important job is creating a new routine that works for you.